
All About the Sesamoids: Patellar Tendonitis and More
Treatment GuidelinesIf you’ve treated patients with patellar tendonitis, then you know the sesamoids in the knee. The smaller sesamoid bones of the hand and feet play a big role in other conditions, but they’re often overlooked. Let’s explore the anatomy, function, and rehab techniques for sesamoid bones.
The human body is comprised of 206 bones that all support our skeletal system. Even people who haven’t studied anatomy can name a few bones, like the femur, carpal bones, and some can name many more. But, are you familiar with the humble sesamoid bones?
A sesamoid bone is a small round bone that is imbedded within a tendon, whose purpose is to reinforce and decrease stress on that tendon. You will mostly find sesamoid bones in the knee, thumb, and big toe1. Others in the hand and feet are much smaller.
If you’ve treated patients with patellar tendonitis, then you know the sesamoids in the knee. The smaller sesamoid bones of the hand and feet play a big role in other conditions, but they’re often overlooked. Let’s explore the anatomy, function, and rehab techniques for sesamoid bones.
Sesamoid in the Knee: The Patella
The most easily found sesamoid bone is the patella, or the kneecap. It is embedded within the patellar tendon that attaches the quadriceps to the tibia. The patella provides an extra mechanical advantage to the thigh, helping extend the knee the last 30 degrees. It guides the knee properly into a flexed position2.
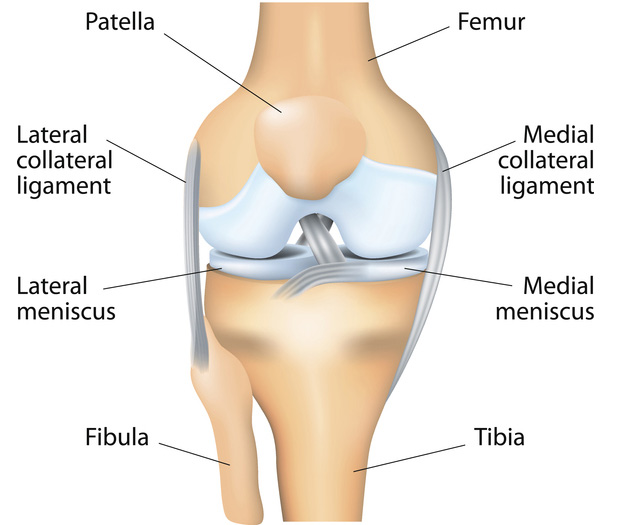
Knee pain is one of the most common complaints of the lower extremities. People of all ages may experience discomfort and injury in the knee. In many cases, the movement of the patella is a primary cause of this discomfort. It’s typically easy to diagnose an inflamed patella, but not necessarily so easy to treat it.
Treating Patellar Tendonitis
Treating an inflamed patella (patellar tendonitis) can be complex. Any one of countless biomechanical factors could cause discomfort. These factors vary from person to person, making each case different from the next.
Generally, a practitioner will start by addressing the most common factors that lead to patellar tendonitis. These include foot mechanics when walking: posture, hip position, knee angle, and other factors that could lead to stress. Once you find the primary biomechanical weakness, you can continue with the appropriate therapeutic intervention.
Many therapists recommend closed-chain eccentric exercise for patellofemoral pain. The eccentric phase of muscle contractions loads the muscle and tendon without placing excessive force on the knee joint or patella.
For example, the Eccentron is a closed-chain, eccentric-only system that gradually loads the entire lower kinetic chain. Dosing is an important part of this intervention and a clinician can choose to increase or decrease the load based on a client’s status. Clinicians have long valued the benefit of eccentric exercise and recently, it has gained even more attention for treating weakened or injured tendons.
Watch this video to see how the Eccentron can restore strength to deconditioned lower extremities.
After repetitive training, the tendon becomes stiffer, and can provide better force control of the patella during walking and running. Exercise with the correct biomechanics is key to long-term success for patellar tendonitis patients.
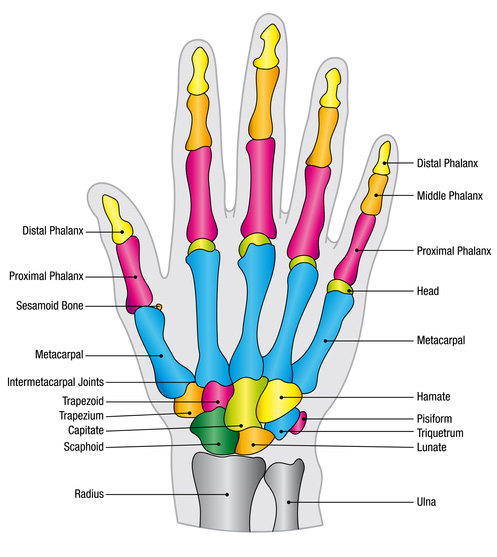
Small Sesamoids in the Hand
In addition to the knee, you can also find sesamoid bones in the hand. Most people have five hand sesamoids. The most common hand sesamoids are two small bones that start at the base of the thumb (distal aspect of the first metacarpal).
Injury to these bones can be difficult to diagnose. Therefore, research articles and case studies rarely feature sesamoids of the hand3. However, these small bones shouldn’t be overlooked as a potential cause of pain or decreased function.
Rehab for Hand Sesamoid Injuries
Patients with upper extremity injuries or surgery often need multiple therapy sessions to make a full return to function without pain. Because hand injuries can significantly impact daily life, it’s important to make a full recovery as safely and effectively as possible.
Treatment for an injured hand sesamoid depends on the cause, whether it’s sudden injury or chronic overuse. Usually, patients need to undergo surgery and other methods to reduce pain, as well as bracing/splinting and exercise. Before surgery, it’s best to complete prehab sessions to strengthen and train the muscles for better recovery.
Start by addressing the isolated movement of the hand and wrist. Once the patient masters isolated movements, you can then move on to integrating functional tasks to restore normal use.
During the isolated movement phase, it’s common to practice grip and pinch exercises. These should focus on isometric contractions and muscle control for the first few sessions. Then, the patient can move on to concentric and eccentric exercise, at a submaximal level.
The Simulator II and PrimusRS systems offer the capability of working small isolated hand movements in the three primary phases of contractions: isometric, concentric, and eccentric. Transitioning from isolated to functional exercises ensures that the patient is capable of doing more complicated tasks, pain free. When strength and endurance improve, the return to function assessment consists of multi-dimensional movements through multiple planes.
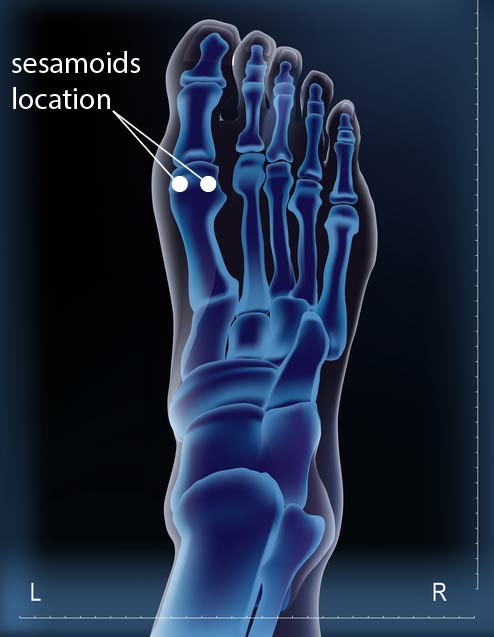
Sesamoids in the Foot: Tibial and Fibular
Lastly, and certainly not least, are the most common sesamoids of the foot. Located in the big toe, these are the tibial sesamoid (on the medial plane) and fibular sesamoid (on the lateral plane).
These two small bones act as a typical tendon support, but they also bear weight and stress. They help transfer force while standing, walking, running, dancing, or jumping.
Though they are incredibly important to function, these their injuries are difficult to diagnose accurately4. As a result, some patients unfortunately receive ineffective recommendations and treatments.
Rehab for Tibial and Fibular Sesamoids
When a patient has pain or injury in the big toe, you can bet that it probably involves one of the two sesamoids. Some call this inflammation “turf toe,” though this term may be more specific to the bony structure and not the soft tissue surrounding the area.
Inflammation of the tibial or fibular sesamoid can create both short- and long-term discomfort, and negatively impact the patient’s activity level. Tightness in the ankle and calf can also contribute to stress around the foot sesamoids. Therapists should address this early on in the intervention process.
Other factors that contribute to a foot sesamoid injury include a person’s gait pattern, shoe wear, weight, lifestyle, and general foot care.
If the sesamoid bone fractures, the patient may need surgery to remove the bone fragments. The surgeon will attempt to leave as much of the sesamoid intact in order to prevent future stress and the formation of bunions. Although it’s not most people’s first choice, surgery can effectively alleviate some patients’ long-term discomfort.
If there is no fracture, or following sesamoid surgery, rehab therapists have many options for treating an injured foot sesamoid. Rehab should include pain management, taping, bracing, calf stretching, and recommending orthotic shoes (firm sole). And, of course strengthening of the structures surrounding the injury and addressing any deficits within the kinetic chain are always recommended.
Every bone in the human body plays a role in the efficient and safe movement in our day to day lives. The larger bones tend to be the more widely known but it is these smaller support structures that can be easily overlooked for their importance. Neglecting discomfort in the sesamoids can lead to more serious issues in the joints, ligaments, tendons, and muscles. These structural issues can lead to decreased function and job and athletic performance if not treated properly.
Hand-held Anatomy Reference Tool
If you need a refresher on muscle movements and nerve innervation, check out the Muscle Joint Action Guide (MJAG), a hand-held anatomy reference tool from BTE. For both upper and lower extremities, it’s the last resource for muscle groups, joint movements, and innervation you’ll ever need.
Jeffrey Johnson, MA, ATC
Clinical Specialist
BTE
References
- Betts, Gordon J, et al. Anatomy and Physiology. BC Open Textbook Project. Chapter 6.3: https://opentextbc.ca/anatomyandphysiology/chapter/6-3-bone-classification/
- Loudon, Janice. Biomechanics and Pathomechanics of the Patellofemoral Joint. International Journal of Sports Therapy. 2016 Dec: 11(6): 820-830. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5095937/
- Dauwe J, Frederic V. Case Report: Oblique Fracture of the Ulnar Sesamoid Bone of the MCP Joint, a Rare Pathology. JOCR, 2017 Mar: 7: p 29-32. http://www.jocr.co.in/wp/2017/03/10/2250-0685-736-fulltext/
- Xiazhong Li, Lenian Shi, Taiyun Liu, Lin Wang. Progress in the clinical imaging research of bone diseases on ankle and foot sesamoid bones and accessory ossicles. Intractable and Rare Diseases Research, 2012 Aug 1(3): P 122-128. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204596/




