Nerve Flossing: Does It Really Work?
Treatment GuidelinesNerve flossing is undoubtedly intriguing, in theory. But how effective is it in practice? Dive into the research on five types of nerve flossing to find out.
Nerve flossing* is a catchy name for a treatment technique.
When one hears the term, even with no medical background, one can easily visualize exactly what this treatment consists of. Just like flossing the teeth, flossing a nerve involves the use of alternating tension on each side of the nerve to slide it along its sheath.
But while nerve flossing is undoubtedly an intriguing treatment in theory, how effective is it in practice?
In this article, I’ll provide an overview of the evidence related to nerve flossing so that you can decide whether or not you should utilize it for your patients.
*Note: I will use the terms “nerve flossing” and “nerve gliding” interchangeably in this article. Some clinicians differentiate between these terms slightly, but for our purposes, both terms refer to the same type of treatment.
Additionally, there are a variety of nerve gliding descriptions in the literature; from very specific guidelines for body position, to very vague parameters. I’ll aim to be as specific as possible when describing the techniques.
Nerve Flossing Overview
There are a few different methods of nerve flossing utilized by clinicians. In general, nerve flossing consists of tensioning the nerve on one end, while relaxing it on the other, alternating the tension between sides throughout the session.
The theory behind this treatment is that the motion releases any restrictions affecting the nerve by slowly gliding the nerve back and forth within its sheath. Often, clinicians use nerve flossing for peripheral nerve injuries, radiculopathies, and other conditions related to the nervous system. For instance, many practitioners rely on nerve flossing as an integral part of their treatment plan for sciatica.
In the following sections, we’ll investigate nerve flossing for specific areas of the body and attempt to determine if the treatment is worth consideration for your practice.
Nerve Flossing for the Upper Extremities
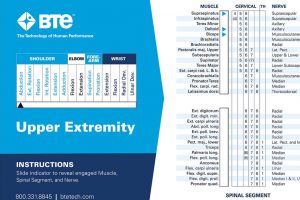
When it comes to the upper extremities, the main structures treated with nerve flossing are the median, ulnar, and radial nerves. Each of these nerve glides requires a specific movement of the upper extremities. The patient may perform the movement on his own, or the clinician may help, depending on the individual situation.
Median Nerve Flossing
Gliding of the median nerve is often part of a treatment plan for those with carpal tunnel syndrome (CTS). Alternatively, the clinician may prescribe this treatment for those who simply have symptoms observed during median nerve tension testing.
To floss the median nerve, the patient assumes a position of:
- Shoulder abduction to slightly less than 90 degrees
- Supination of the wrist
- Elbow extension
- Wrist extension
- Depression of the involved scapula
- Lateral cervical flexion to the involved side
From this starting position, the patient laterally flexes their head to the opposite side as they flex the wrist. They’ll hold this position momentarily, then returns to wrist extension and ipsilateral cervical sidebending. The patient repeats this alternating movement pattern throughout the exercise.
Evidence for Median Nerve Flossing
In 2015, researchers conducted a systematic review of randomized controlled trials on the available evidence for median nerve flossing for carpal tunnel. This review concluded that, when median nerve flossing was combined with conventional CTS treatments, patients seemed to do better than compared to conventional care alone.1
Another review from 2017, however, demonstrated little benefit of nerve flossing for most conditions, including carpal tunnel syndrome.2
Ulnar Nerve Flossing
Flossing of the ulnar nerve may be included in treatment plans designed for cubital tunnel syndrome or other conditions affecting the ulnar nerve.
To glide the ulnar nerve, the patient assumes a position of:
- Shoulder abduction to slightly less than 90 degrees
- Pronation of the wrist
- Elbow flexion
- Wrist extension
- Depression of the involved scapula
- Lateral cervical flexion to the involved side
Once positioned as described, the patient then laterally flexes their head to the contralateral side as they simultaneously flex the wrist. They maintain this position momentarily, then returns to the original position outlined above. They will alternate between these positions throughout the exercise.
Evidence for Ulnar Nerve Flossing
A 2022 review found that ulnar nerve mobilization seems to be effective for ulnar neuropathy at the elbow. However, the clinician should note that some of the studies included in the review did not show strong evidence for this treatment option, and some of them were not high quality studies in general.3
Radial Nerve Flossing
Radial nerve entrapment is quite rare. Usually, issues affecting the radial nerve are due to trauma, such as a humeral fracture. Therefore, this is not typically a go-to treatment option for many clinicians.
In order to glide the radial nerve, the patient assumes a position of:
- Shoulder abduction of 5-10 degrees
- Slight internal rotation of the involved shoulder
- Depression of the involved scapula
- Elbow extension
- Wrist flexion
- Cervical sidebending to the involved side
In order to perform the flossing motion, the patient bends their head to the contralateral side and simultaneously extends the wrist. They will hold this position momentarily, then returns to the starting position. The patient alternates between these two positions for the number of prescribed reps.
Evidence for Radial Nerve Flossing
A small study from 2014 found that lateral elbow pain was reduced through the use of radial nerve mobilizations.4
Unfortunately, few other studies have examined radial nerve flossing at all. Other studies that looked at this treatment option were part of general evaluations of neural mobilizations, and they didn’t examine radial nerve flossing very closely.
Nerve Flossing for the Lower Extremities
When it comes to nerve gliding for the lower body, two main nerves bear consideration: the sciatic nerve and the femoral nerve.
Both the sciatic nerve and the femoral nerve are targets of nerve flossing, especially in cases of low back pain.
Sciatic Nerve Flossing
Seeing as the sciatic nerve is the longest nerve in the body, gliding this structure requires near-total body movement. In order to floss the sciatic nerve, the patient is usually seated, assuming a position of:
- Cervical flexion
- “Slumped” thoracic spine
- Knee flexion
- Slight plantar flexion
When instructed, the patient extends the knee and dorsiflexes the ankle while extending the cervical spine. Alternate between these two positions, holding each briefly for each rep of the exercise.
Evidence for Sciatic Nerve Flossing
In multiple studies, researchers demonstrated a benefit of implementing sciatic nerve flossing.** As stated earlier, most of the time, practitioners use these treatments for cases of low back pain with radiating leg symptoms.5, 6
**Note: some of these studies used slightly different gliding techniques than the one described above.
Femoral Nerve Flossing
Of all the nerve glides described in the literature, the femoral nerve glide likely has the most variability in terms of technique. For this nerve glide, the patient may maintain a position in prone, sidelying, or even in sitting. I will describe the prone version.
The patient assumes a position of:
- Lying prone
- Cervical extension
- Knee flexion
- Ankle plantarflexion
From this position, the patient extends the knee while simultaneously flexing the cervical spine. Alternate between these two positions throughout the exercise.
Evidence for Femoral Nerve Flossing
A study of hemophilic patients with femoral neuropathy found that femoral nerve flossing was effective for reducing pain and improving function.7
Outside of this study, most of the evidence on nerve gliding for the femoral nerve comes from research on the general effect of nerve flossing as a treatment option.
Should You Add Nerve Flossing to Your Repertoire?
Based on the available evidence, nerve flossing appears to be a safe, effective treatment for a variety of conditions. However, there are also plenty of other treatment modes that work well for low back pain, carpal tunnel syndrome, and other conditions mentioned in this post.
So, should you include nerve flossing in your treatment toolbox?
If you’re having success treating nerve conditions and other issues without the use of nerve flossing, there is probably no reason to switch things up. However, if you have a tricky patient for whom none of your usual treatments are relieving their symptoms, you may consider gliding their involved nerves.
Again, when performed conservatively, the treatment poses little risk to the patient, and it may benefit them. Further, the benefits of trialing the treatment will often outweigh the risks.
Bennett Richardson, PT, DPT, CSCS
Bennett Richardson, PT, DPT, CSCS is a physical therapist and writer. He is the owner of Richardson PT LLC, a mobile, cash-based physical therapy service out of Pittsburgh, PA. Ben is passionate about many health-related topics including weight loss and athletic performance. To get in touch with Ben, visit www.richardsonpt.com
References
- Kim S. D. (2015). Efficacy of tendon and nerve gliding exercises for carpal tunnel syndrome: a systematic review of randomized controlled trials. Journal of physical therapy science, 27(8), 2645–2648. https://doi.org/10.1589/jpts.27.2645
- Basson, A. et al. (2017) “The effectiveness of neural mobilization for neuromusculoskeletal conditions: A systematic review and meta-analysis,” Journal of Orthopaedic & Sports Physical Therapy, 47(9), pp. 593–615. Available at: https://doi.org/10.2519/jospt.2017.7117.
- Poenaru, D., Ojoga, F., Sandulescu, M., & Cinteza, D. (2022). Conservative therapy in ulnar neuropathy at the elbow (Review). Experimental and therapeutic medicine, 24(2), 517. https://doi.org/10.3892/etm.2022.11444
- Arumugam, V., Selvam, S., & MacDermid, J. C. (2014). Radial nerve mobilization reduces lateral elbow pain and provides short-term relief in computer users. The open orthopaedics journal, 8, 368–371. https://doi.org/10.2174/1874325001408010368
- Jeong, U. C., Kim, C. Y., Park, Y. H., Hwang-Bo, G., & Nam, C. W. (2016). The effects of self-mobilization techniques for the sciatic nerves on physical functions and health of low back pain patients with lower limb radiating pain. Journal of physical therapy science, 28(1), 46–50. https://doi.org/10.1589/jpts.28.46
- Alshami, A. M., Alghamdi, M. A., & Abdelsalam, M. S. (2021). Effect of Neural Mobilization Exercises in Patients With Low Back-Related Leg Pain With Peripheral Nerve Sensitization: A Prospective, Controlled Trial. Journal of chiropractic medicine, 20(2), 59–69. https://doi.org/10.1016/j.jcm.2021.07.001
- Hamed, S. A., Zoheiry, I. M., Waked, N. M., & Saad El-Din Mahmoud, L. (2021). Effect of Neurodynamics Nerve Flossing on Femoral Neuropathy in Haemophilic Patients: A randomized controlled study. Journal of musculoskeletal & neuronal interactions, 21(3), 379–386.