
Guide for Workers' Comp Rehabilitation: Driving Revenue, Outcomes, and Efficiency
Treatment GuidelinesLearn how to create effective workers’ comp rehab programs that improve return-to-work times, enhance documentation, and drive strong clinical and financial results.
Workers’ compensation rehabilitation success requires more than traditional therapy approaches. Modern clinics are building comprehensive programs on three pillars: clinical specialization, objective data, and operational efficiency. This playbook shows you how to evolve from basic return-to-work services to a data-driven program that improves patient outcomes, streamlines reimbursement, and differentiates your practice.
Key strategies include implementing evidence-based protocols, using objective functional testing, developing specialized work conditioning programs, and leveraging technology for superior documentation that satisfies all stakeholders.
Beyond the Basics of Return-to-Work
Every stakeholder in a workers’ compensation case shares the same goal: achieving a safe, timely, and durable return to work. Yet if you’re managing a rehab clinic or directing a work comp program, you know that reaching this goal consistently and profitably has become increasingly complex.
Traditional therapy approaches often result in delayed timelines, subjective progress notes that fail to convince adjusters, and endless reimbursement battles. Meanwhile, employers demand faster returns to productivity, insurers require bulletproof documentation, and injured workers need confidence that they can return to their jobs without re-injury.
The most successful clinics are evolving beyond these challenges. They’re building comprehensive work comp programs founded on three essential pillars: clinical specialization, objective data, and operational efficiency. This article provides your playbook for implementing that system, transforming your workers’ comp services from a challenging revenue stream into a profitable center of excellence.
Aligning Stakeholder Goals
The Business Case for Employers and Payers
Let’s move beyond the simple “cost reduction” argument. What employers and payers really need is strategic risk management through predictable, measurable outcomes. Yes, reducing lost work time and lowering compensation costs matter, but what sets apart a premier workers’ comp rehab program is its ability to provide clarity and confidence in decision-making.
When you implement a structured rehabilitation program with objective measurement capabilities, you’re offering something invaluable: predictability. Payers can close claims with confidence because they have clear, defensible data showing functional improvement. Employers can make informed decisions about modified duty assignments because they understand exactly what physical demands their employee can handle.
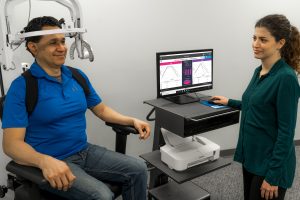
Consider how tools like the PrimusRS help clinicians provide multi-joint functional rehabilitation with objective strength assessment. This isn’t just about measuring progress; it’s about creating a shared language of functional capability that all stakeholders understand and trust.
The Human Case for the Injured Worker
While financial metrics drive business decisions, we can’t forget the human element that ultimately determines success. Injured workers face not just physical challenges but also financial stress and uncertainty about their future. A clear, goal-oriented rehabilitation program with visible progress measurements builds patient confidence and engagement.
When patients can see objective improvements in their functional capacity week by week, it transforms their mindset from “Will I ever get better?” to “Look how far I’ve come.” This psychological shift directly impacts adherence rates and, ultimately, outcomes. Your role is to create an environment where progress is measurable, achievable, and clearly communicated.
Clinical Excellence and Coordinated Care
Building on Evidence: Adhering to Treatment Guidelines
Adherence to established treatment guidelines like ODG (Official Disability Guidelines) and state-specific protocols isn’t just about compliance; it’s your roadmap to clinical efficiency and cleaner reimbursement. These guidelines provide evidence-based benchmarks that help you set realistic expectations and justify your treatment plans.
For example, research indicates that soft tissue injuries typically require 6 to 12 visits, while post-surgical cases may need 12 to 24 visits.1 Understanding and documenting your adherence to these benchmarks positions your clinic as a responsible steward of healthcare resources while providing the framework for efficient care delivery.
Think of guidelines as guardrails that keep your treatment on track while providing the documentation backbone that adjusters and case managers need to approve continued care. When you can show that your treatment aligns with established protocols and that you’re measuring functional progress objectively, reimbursement discussions become much smoother.
The Power of Case Management
Case managers serve as the air traffic control for the rehabilitation process, coordinating between multiple providers, employers, and insurers. Your success in workers’ comp rehab often depends on how effectively you partner with these crucial stakeholders.
The key to this partnership? Providing case managers with clear, objective, functional data rather than subjective reports. When you can demonstrate through tools like the EvalTech system that a patient has achieved specific functional milestones matched to their job demands, you make the case manager’s job easier and position your clinic as a preferred provider.

Specialized, Job-Specific Rehabilitation Programs
From Acute Care to Functional Restoration
The journey from injury to return-to-work follows a predictable progression, and understanding each phase allows you to deliver targeted, effective interventions. Initial physical and occupational therapy focuses on restoring range of motion, managing pain, and rebuilding foundational strength. But this is just the beginning.
As patients progress, the focus must shift from general conditioning to job-specific functional restoration. This is where many clinics fall short, continuing with generic exercises when what the patient really needs is task-specific training that prepares them for their actual work demands.
Bridging the Gap: Work Conditioning vs. Work Hardening
Understanding when and how to implement specialized programs separates comprehensive workers’ comp providers from generalist clinics. Work conditioning programs, typically running 2 to 4 hours per day, focus on restoring physical capacity for workers with moderate job demands. These programs emphasize general conditioning, flexibility, and coordination while beginning to introduce job-simulated activities.
Work hardening takes this further, offering 4 to 8 hours of intensive, job-specific training for workers with heavy physical demands. Here, you’re not just building strength; you’re recreating the actual tasks, postures, and endurance requirements of the patient’s job. Systems like the Simulator II help clinicians replicate job tasks and activities of daily living while capturing objective documentation of performance.

These specialized programs represent a high-value service line that differentiates your clinic from competitors while providing objective justification for continued care. When an adjuster questions why additional therapy is needed, you can demonstrate exactly how your program is preparing the worker for the specific demands they’ll face upon return.
The Central Role of Objective Data and Superior Documentation
Moving Beyond Pain Scales: The Shift to Functional Outcome Measures
Pain scales have their place, but they tell only a small part of the story. Modern workers’ comp rehabilitation demands functional outcome measures that directly relate to job performance. Can the worker lift 50 pounds from floor to waist? Can they maintain overhead positioning for extended periods? Can they demonstrate the endurance needed for an 8-hour shift?
Objective functional testing removes the guesswork from return-to-work decisions. When you document a worker’s ability to perform job-specific tasks at required frequencies and durations, you’re providing legally defensible data that protects both the employer and the employee from premature return-to-work decisions.
The Technology Advantage: Tools for Objective Measurement
Technology has transformed our ability to capture and communicate functional progress. Modern evaluation systems provide micro-motion analysis and real-time feedback that turns subjective observations into quantifiable data. For instance, the Prism system delivers high-precision functional testing in a compact format, perfect for clinics where space is limited. Portable testing tools like EVJ and the Evaluator expand your clinic’s services to jobsite evaluations.
These tools aren’t novelties; they’re essential instruments for capturing the functional data that drives modern workers’ comp programs. They provide objective proof of progress or plateaus, helping you make data-driven decisions about treatment continuation or discharge readiness.
Documentation that Drives Reimbursement and Communication
Translating objective data into compelling documentation is an art form that directly impacts your reimbursement rates and stakeholder relationships. Your documentation should tell a clear story of functional improvement that connects treatment activities to job-specific gains.
Consider this documentation framework: Start with the initial functional status, describe the specific treatment activity performed, document the objective functional gain achieved, and explicitly link this improvement to a specific job demand. For example: “Patient initially demonstrated 15-pound lift capacity from floor to waist. Following progressive resistance training using objective testing equipment, patient now demonstrates 35-pound lift capacity, meeting the medium-duty work requirement for their warehouse position.”
This approach transforms your documentation from a clinical note into a powerful communication tool that speaks directly to the concerns of employers, adjusters, and case managers.
Managing Complex Cases and Standardizing Systems
A Modern Approach to Catastrophic Injuries
Complex injuries require sophisticated management strategies that go beyond traditional therapy approaches. Effective management of catastrophic cases demands a multidisciplinary team armed with objective progress data and clear communication protocols. Systems like the Multi-Cervical Unit enable clinicians to provide specialized cervical evaluation and strengthening with the objective data necessary for managing complex neck injuries.
The key is building a systematic approach where every team member understands their role, progress is measured objectively across all domains, and communication flows seamlessly between providers, case managers, and stakeholders.
Standardization for Growth and Quality
As your workers’ comp program grows, standardization becomes crucial for maintaining quality while improving efficiency. Evidence-based protocols and technology platforms allow you to standardize care across multiple sites and practitioners, ensuring consistent quality regardless of who delivers the service.
This standardization simplifies training for new staff, provides administrators with system-wide data for performance analysis, and creates predictable outcomes that strengthen your relationships with referral sources. When every therapist in your organization follows the same evidence-based protocols and uses the same objective measurement tools, you create a reliable, scalable system that can grow with demand.
Conclusion: Becoming the Go-To Workers’ Comp Provider
We’ve journeyed from understanding why workers’ comp rehabilitation matters to mastering how to build a comprehensive, profitable program. The modern work comp provider isn’t just a service vendor; you’re a data-driven partner who helps all stakeholders achieve their goals through clinical excellence and objective measurement.
For clinic owners, this approach means increased revenue through specialized service lines, market differentiation through superior documentation, and operational efficiency through standardized protocols. Work comp directors gain defensible return-to-work decisions and stronger relationships with employers and payers. Clinicians experience greater confidence in their clinical decisions and enhanced patient outcomes. And administrators benefit from system-wide compliance and data-driven management capabilities.
Ready to transform your workers’ comp program from a cost center to a center of excellence?
Discover how BTE’s comprehensive suite of evaluation and rehabilitation systems can help you build a more profitable and effective practice. Our tools for objective testing, functional rehabilitation, and streamlined documentation provide the foundation for a modern workers’ comp program that satisfies all stakeholders while driving superior outcomes.
The future of workers’ comp rehabilitation belongs to those who embrace objective measurement, evidence-based protocols, and stakeholder-focused communication. With the right approach and tools, you can position your clinic as the preferred partner for employers, insurers, and injured workers alike.
Workers’ Compensation Rehabilitation FAQs for PT & OT Clinic Staff
Q1: How many therapy visits are typically approved for workers’ compensation cases?
A: Visit authorization depends on injury complexity and state guidelines. Uncomplicated soft tissue injuries typically receive 6-12 visits over 4-6 weeks, post-surgical cases may get 12-24 visits over 8-12 weeks, and complex multi-injury cases can require 18-30 visits over 12-16 weeks. Always verify specific authorization limits with the insurance carrier and follow state-specific protocols like the 24-visit limitation in California for PT, OT, and chiropractic care.
Q2: What’s the difference between Work Conditioning and Work Hardening programs?
A: Work Conditioning is designed for workers with sedentary to medium physical job demands, involving 2-4 hours per day, 3-5 days per week, focusing on basic strength, flexibility, and endurance. Work Hardening is for workers with medium to very heavy physical demands, requiring 2-8 hours per day, 3-5 days per week, and includes real and simulated work activities specific to the patient’s job duties. Work Hardening is more intensive and job-specific.
Q3: What documentation is required to justify continued treatment in workers’ comp cases?
A: Documentation must demonstrate specific functional improvements, not just pain reduction. Include objective measurements (strength, ROM, work-specific tasks), show decreasing reliance on passive treatments over time, and clearly link treatment activities to return-to-work goals. Progress notes should reflect movement toward functional outcomes like job-specific task performance, work endurance, and psychosocial readiness. Any deviations from expected progress require clear clinical rationale.
Q4: How should treatment frequency change throughout the rehabilitation process?
A: Treatment typically starts at 2-3 visits per week during acute phases, then decreases to 1-2 visits per week as patients gain independence. The progression should move from passive treatments to active rehabilitation, then to work-specific conditioning. Eventually, patients should transition to independent home exercise programs. This progression should be documented and justified based on functional improvements and return-to-work goals.
Q5: What are the key outcome measures we should focus on for workers’ comp patients?
A: Focus on functional outcomes rather than impairment measures. Key areas include: ability to perform specific job tasks, endurance and tolerance for work activities, psychosocial readiness to return to work, and objective measures of strength/ROM related to job demands. Document improvements in work-specific activities like lifting capacity, prolonged sitting/standing tolerance, repetitive motion capability, and overall confidence in performing job duties safely.
Q6: What are our responsibilities regarding return-to-work coordination?
A: Collaborate with case managers, employers, and physicians to facilitate safe return-to-work. Provide detailed functional capacity evaluations when requested, communicate any work restrictions or accommodations needed, and ensure treatment plans align with job demands. Document all communications regarding return-to-work status, participate in team conferences when requested, and provide objective assessments of the patient’s readiness to resume specific work duties without risk of re-injury.






