
Occupational Therapy Aids for Elderly Clients: A Guide for OTs
Treatment GuidelinesExplore effective OT aids for elderly patients. Enhance safety, independence, and daily function with expert guidance for therapists.
As occupational therapists, we love helping to facilitate independence with practical adaptive aids. When we think of occupational therapy for elderly clients, we have to consider certain nuances to make sure we’re recommending products that are appropriate, easy to use, and multi-purpose when possible.
As our clients age, various degrees of cognitive decline can affect how they learn, use, and adapt to changes in function and their environment. In my personal practice, this directly affects what and when I recommend certain products, when I involve family in self-care tasks, and helps me suggest appropriate adaptations moving forward.
The Role of Occupational Therapy Aids in Elderly Care
Assistive and adaptive equipment is designed to facilitate independence and support an individual’s dignity, without being a crutch. Depending on the circumstances, some devices may be used intermittently, temporarily, or permanently. The goal is to always recommend aids that are simple to use and help our clients maintain independence and dignity, even as their abilities change. The last thing we want is to give our clients something they won’t use, find frustrating, or make them feel less dignified.
How Sound Recommendations Keep Seniors Independent
Recommending appropriate occupational therapy equipment for elderly clients is key to keeping seniors independent without overburdening them with glorified knick-knacks. Of course, there are hundreds of products and adaptations to make self-care and home tasks much easier. But many are not completely necessary for all clients, so it’s important to be judicious in our recommendations. When I recommend products, I want to make sure they’re enhancing my client’s overall safety and preventing falls whenever appropriate.
For example, if a client just had a hip replacement and their hip precautions limit them from bending over to put on their pants, a reacher or dressing stick could help them through this temporary limitation.
Another example would be a client with advancing dementia who is slowly losing strength and flexibility to lift themselves off of the toilet, but can still complete toileting hygiene independently. For this client, I would recommend a toilet riser or a 3-in-1 commode to place over the toilet to add extra height for safety and falls prevention, and this would likely be a permanent adaptation.
Each tool serves a purpose, and the decision to introduce one should be guided by a client’s functional needs, goals and long-term safety. With that foundation in mind, we can be more selective in how each recommendation supports aging adults in meaningful, practical ways.
Categories of Assistive Devices
There’s an endless sea of assistive devices to choose from, all of which have a specific purpose, pros and cons, as well as insurance or payment barriers.
ADL equipment: The most common assistive devices I use regularly in practice are equipment for ADLs, including:
- Dressing sticks
- Long handled shoehorns
- Reachers (also called grabbers)
- Sock aids
- Universal cuff
- Build up handles
- Adaptive eating utensils
- Adaptive kitchen equipment
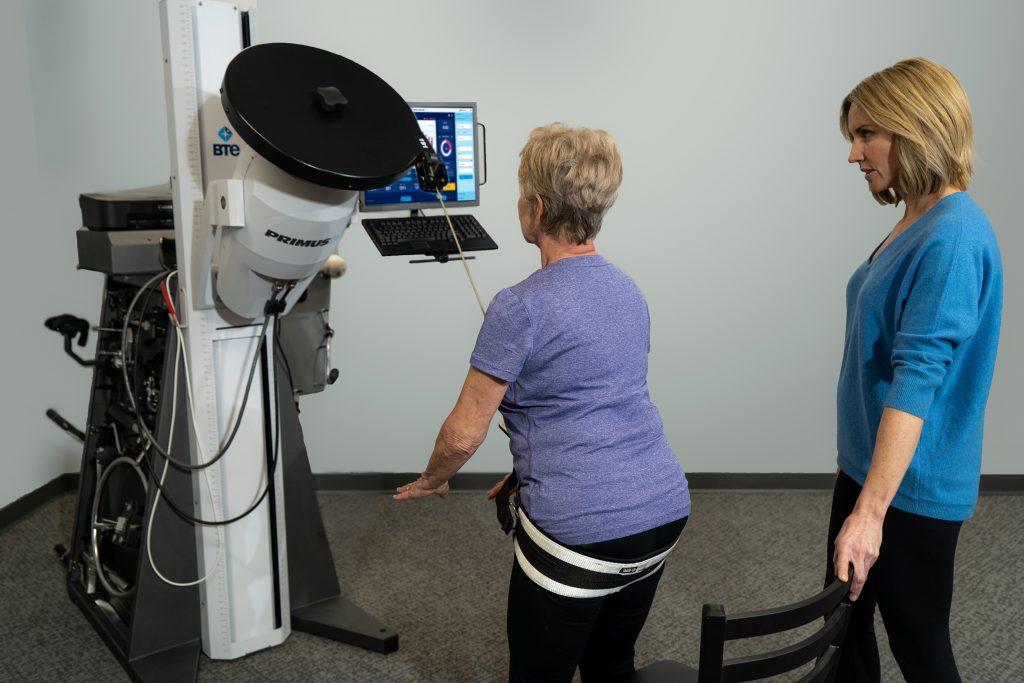
Professional-grade equipment like PrimusRS and Simulator II allow clinicians to simulate ADLs and common functional tasks in the clinic. A variety of handles, tools, and attachments make every activity adaptable to individual needs and abilities.

Mobility aids: Other assistive devices and durable medical equipment in the mobility aid category, include:
- Various types of walkers
- 3-in-1 commodes
- Shower chairs or tub transfer benches
- Specialty shower chairs or rolling shower chairs
- Canes or hemi walkers
- Visibility tape, certain types of lighting
- Grab bars or railings
Cognitive support tools These are tools that support various higher-level cognitive functions that often decline as people age. These can include:
- Electronic or paper calendars
- Traditional pill organizers
- Electronic pill dispensers
- Smartphone apps for reminders to take medications, pressure relief, or even hydrate
OT Aid Selection and Assessment Process
Living safely and confidently is one of the most frequent goals I see in senior occupational therapy. Effective implementation and training of adaptive tools is often the other half of that puzzle. Combined with neuromuscular reeducation and functional rehabilitation activities tailored specifically for seniors, this makes a comprehensive approach to occupational therapy for the elderly.
Patient-Centered Assessments Help Give a Comprehensive Picture
A truly patient-centered assessment involves understanding the person as a whole and how their health impacts their daily life. Occupational therapy assessments begin by evaluating functional and cognitive abilities, which determines how well a client can complete ADLs. Equally important is performing a home safety evaluation, to examine the client’s living environment for hazards and opportunities for adaption.
The AMPS1 is one of my favorite standardized assessments to incorporate for assessing motor skills, cognition, and overall safety awareness. For clients experiencing cognitive decline, it’s also helpful to pair with other cognitive assessments like the interview of deterioration in daily activities in dementia (IDDD) to see how a patient’s performance impacts caregiver burden2.
Matching OT Aids to Specific Conditions and Financial Hurdles
Occupational therapy aids are often multi-purpose, but it’s important to consider specific client factors when making these recommendations, and to specifically document them in your clinical notes. Joint replacements, spinal fusions, even debility can all benefit from the same piece of equipment but for different reasons.
For example, I’ll often recommend reachers to prevent falls or prevent certain movements, according to the post-surgical precautions. To justify this piece of equipment, my notes might look something like this:
| Client A, status post total hip arthroplasty with posterior hip precautions | Client requires <75% assistance with lower body dressing tasks to thread bilateral feet and legs through pants and underwear 2/2 posterior hip precautions limiting ROM. Client educated on use of reacher for lower body dressing tasks. Client demonstrated use of reacher to don pants and completed with supervision only while adhering to posterior hip precautions. |
| Client B, status post T10-L1 instrumented fusion. | Client requires >75% assistance with lower body dressing 2/2 spinal precautions limiting ability to bed to feet in sitting and supine. Client educated on use of reacher for lower body dressing tasks and demonstrated use of reacher to don pants with supervision only while adhering to spinal precautions. |
| Client C, history of beginning stages of dementia, status post hospital stay for debility | Client demonstrates posterior lean and a need for intermittent minimal assistance (25%) for dynamic sitting balance at edge of bed. Client requires moderate (<50%) assistance to don pants 2/2 balance deficits. Client educated on use of reacher for lower body dressing tasks and with moderate verbal cues, able to demonstrate needing <25% of assistance for these tasks. Recommend continued repetition with this tool to increase independence with routine adaptations. |
Navigating Financial and Insurance Hurdles
Not all equipment will be covered by insurance, and reimbursement cuts are being made left and right, so it’s best to document why an aid is medically necessary to support your client’s goals.
Recently, I have had to shift my client education based on the lack of insurance reimbursement for certain equipment. For example, Medicare no longer covers shower DME, including tub transfer benches or shower chairs. Many insurance companies also do not cover padded commodes or shower chairs (which are often necessary for skin integrity maintenance), and some further deny reimbursement for a bedside commode if a patient is issued a rolling walker.
Many elderly clients are on a fixed income, and it’s important to consider their budget if they need to pay out of pocket for DME. Many yard sale groups, second-hand stores, or friendly neighbors may have a lightly used bedside commode or shower chair that can be easily sanitized.
For others who can afford the sticker price for DME, I always advise them to review online listings carefully and shop around if necessary for the best price with practical features. Ultimately, there needs to be a balance between function and price regardless of the financial situation.
Effective Implementation and Training
Hands-on demonstration and practice sessions are some of the best ways to help clients understand and get used to using their new equipment.
Overcoming Resistance and Ensuring Compliance
Some clients may resist using any equipment because of a perceived stigma of “getting old”. In these cases, I find that once a client experiences how much the equipment can help them, they immediately abandon that stigma and appreciate their new level of independence.
Training for Clients with Cognitive Decline
For patients experiencing cognitive decline, I involve the family much more closely. I educate the family on how my client’s current cognitive function affects their independence and safety, how to adapt to changes as they arise, and seeking community resources.
It’s important to remind elderly clients that the need for a physical or cognitive aid isn’t tied to their intelligence or worth. Aging can naturally bring changes in memory, processing speed, or executive functioning. Framing occupational therapy aids as helpful partners rather than signs of weakness helps preserve dignity and encourages clients to accept support without shame.

Overwhelmed Caregivers Need You Too
Another strategy to help clients get used to their new devices is involving family or caregivers. As OTs, we wear a lot of hats, and sometimes that hat is being a listening ear and a voice of reason for family and caregivers. In my experience, listening to family’s concerns and feelings about their loved one opens the door to more effective collaboration.
After validating those thoughts and fears, I explain my rationale behind the equipment recommendations. Training the family focuses on not only how I assess products, but also helping them evaluate products methodically to avoid getting overwhelmed. Helpful points to cover include:
- What features I am specifically looking for in a product and why
- What clues I look for to see if a product is superfluous or overpriced
- Why I would choose one product or feature over others
- Safety considerations of features that otherwise look helpful and easy. For example, I never recommend suction cup handles for the shower or bathtub because they tend to pop off the wall during transfers and cause injuries.
After a few sessions incorporating this approach, I find that the family can methodically browse products more efficiently and calmly because they have a sort of framework to reference.
Monitoring Use and Measuring Outcomes
Occupational therapy aids are only useful if the client incorporates them into their daily life and routines. With more complex tools, follow-up visits in the clinic are beneficial to see how your client actually uses an aid versus how they say they use the aid.
Using systems like the PrimusRS and Simulator II are particularly helpful in measuring outcomes. They’re able to simulate hundreds of activities and ADL tasks, and give quantitative data that can not only measure progress, but justify continued care and adaptive equipment needs for insurance reimbursement.
Integrating OT Aids Into Your Clinic’s Practice
Incorporating occupational therapy aids into your clinic’s practice starts with building a clear and intentional strategy for assessment, implementation, and measuring outcomes. When you identify the most common functional challenges, you can stock a curated selection of high-value and versatile tools that address those needs. Staff and family education regarding aids is equally important for effective training and implementation.
Start with reviewing the durability, material, ease of use, and adjustability of adaptive products, and compare these against other options that may be useful for different kinds of clients. Comparing products side-by-side can also reveal differences in ergonomics, client comfort, and any required maintenance that may impact your decision to stock them in your clinic. At the end of the day, the best OT aids have a balance of performance, usability, and value that support effective, high-quality care.
Ethical Considerations
As healthcare professionals, part of our job is to keep our equipment recommendations appropriate, rather than trying to profit from clients. Ethically, we have to be mindful and diligent in understanding why a more expensive product benefits our clients more than a less expensive option.
Emerging Trends in Assistive Technology
For some seniors, there comes a time when family eventually has to implement some of their own safety measures. Smart home devices or closed surveillance systems are more affordable now than ever, and can be the difference between aging in place for a few more years versus a skilled nursing facility. Wearable fall detection technology is another tool that can add an extra layer of safety and peace of mind.
Conclusion
Empowering our seniors to regain and retain their independence as a way to preserve their dignity is one of my favorite parts of being an occupational therapist. Quality product recommendations paired with functional exercises and interventions are powerhouses to giving elderly clients hope to stay at home longer, and family peace of mind that their loved ones will be safer.
The future of OT aids is likely going to develop with more tech advances, but I think that the tried-and-true simple gadgets like sock aids, reachers, and dressing sticks are going to be around for the long haul. Regardless of how advanced OT aids become, we still have a duty as OTs to account for all parts of our client, what best fits them, their lifestyle, and helps reduce caregiver burden, and what’s financially and cognitively feasible for them.


